Magnets – The New Buzzword in Regenerative Medicine
One of the most promising avenues of regenerative medicine is the injection of intact, living cells into a patient, a branch of medicine known as cell therapy. For instance, as a form of immunotherapy, T-cells may be injected into a patient to fight cancer cells with cell-mediated immunity.
After a therapeutic cell phenotype has been developed, the challenge in cell therapy is to efficiently deliver and retain these cells in the target tissue. Additional hurdles are posed by difficulties in monitoring the therapy in terms of safety and efficacy.
Regenerative Medicine, a bimonthly peer-reviewed journal, reports that magnetic particle tracking could be a potentially revolutionary strategy that will overcome these challenges of disease treatment with cell therapy. The article, written by a group from the UCL Centre for Advanced Biomedical Imaging in London, discusses emerging and established techniques for utilizing magnetic particles to target, image, and activate cells in the human body.
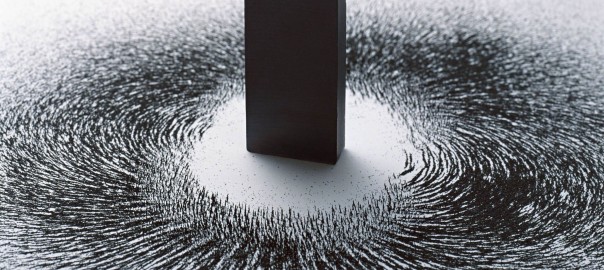
Controlling stem cells magnetically in the body is both fascinating and promising, states Mark Lythgoe, director of the UCL center. Nano-magnets have the potential to guide and stimulate therapies at a microscopic level. The technique also has the potential to combine diagnostics and therapy—a process known as theranostics—for a novel approach to imaging and therapy.
The Division of Cardiovascular Medicine at Stanford University in California has studied the use of magnetic nano-particles to target and image stem cells in the treatment of myocardial infarctions (heart attacks). Heart cells (cardiomyocytes) have limited potential to proliferate and self-heal following injury, and thus, injuries to the myocardium (heart muscle) are often permanent. Cardiac progenitor cells (CPCs) migrate to the site of injury and differentiate into cardiomyocytes to generate new myocardium, but their numbers are limited.
To compensate for the low numbers of CPCs in the injured myocardium, it has been proposed that induced pluripotent stem cells (iPSCs) be therapeutically delivered to generate derived cardiomyocytes and repair the damaged myocardium. The challenge in cardiac stem cell therapy remains in effectively delivering and monitoring the injected cells.
Super-magnetic iron oxide nano-particles (SPIONs) are widely employed in molecular and cellular imaging, and the group at Stanford focused on the use of SPIONs in site-specific delivery and monitoring of stem cells in the treatment of heart attacks.
Nano-particles have several properties that make them especially useful in cell therapy. They are biocompatible, they have magnetic properties, they are amenable to size control, and their surface coating is tailor-made for selective binding, all of which make them ideal for precision biomedical applications, targeted delivery, and in vivo monitoring of injected stem cells. Nanotechnology has a multitude of applications in medicine, cancer treatment, drug delivery, and cell tracking, for example.
Stem cells are a promising treatment for many diseases, especially those currently untreatable or associated with permanent tissue damage. Magnets are the new buzzword in regenerative medicine as a new technique to deliver stem cells to the desired location, monitor them, and discriminate between live and dead cells. This quickly emerging technique holds great potential for clinical application, but further research is needed on the role of SPION-labeled stem cell therapy.
References:
http://www.eurekalert.org/pub_releases/2015-10/fsg-rmg102615.php
https://en.wikipedia.org/wiki/Cell_therapy
http://www.hindawi.com/journals/sci/2016/4198790/
Image courtesy of http://futurism.com/


