New Research into Diabetic Foot Ulcers and Stem Cell Treatment
Researchers at Egypt’s Assiut University are studying the application of stem cell treatment for chronic diabetic foot ulcers. The interventional study, which is not yet open for enrollment, is an open-label single group assessment.
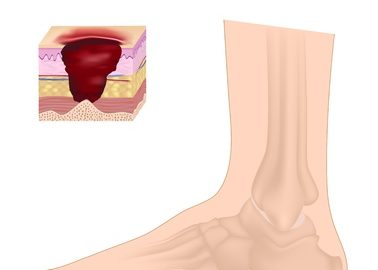
Diabetic Foot Ulcers and Amputations
It is estimated that approximately 15 percent of diabetics develop a foot ulcer at some point during the course of their disease. In the United States, diabetes is the primary cause of non-traumatic amputations of the lower extremities. About 60 percent of diabetics have peripheral neuropathy which results in loss of protective sensation. Diabetics are also prone to atherosclerotic changes in the peripheral arteries. Combined with the anatomy of the foot and the mechanical stresses it is subject to, these conditions predispose diabetics to chronic foot ulcers.
Diabetic foot wounds are staged according to the depth of soft tissue and bony involvement. The traditional treatments for diabetic foot ulcers are offloading the foot, therapeutic footwear, debridement, antibiotic therapy, and saline dressings to keep the wound moist. Peripheral arterial insufficiency is addressed and blood glucose levels are controlled.
Unfortunately, foot ulcers are a significant complication of diabetes that tend to become chronic non-healing wounds. If a person with diabetes develops one ulcer, the chances of developing another ulcer are more. Despite advances in wound care over the past few decades, the outcomes for diabetic foot wounds have not changed substantially. This underscores the need to develop more effective alternative treatments for patients with diabetic foot ulcers.
Stem Cell Therapy for Diabetic Foot Ulcers
Stem cell therapy has shown great promise in wound healing and tissue regeneration. One population of stem cells known as mesenchymal stem cells (MSCs) are multipotent with several clinical applications. MSCs are particularly effective in differentiating into cells originating from the fascia. They are a source of soluble growth factors necessary for tissue regeneration and wound healing. MSCs are present in abundant quantities in adipose (fat) tissue. In fact, adipose-derived pluripotent stem cells are known to secrete factors essential for healing damaged tissue. Moreover, adipose tissue is available in plenty, can be isolated with ease, proliferates extensively ex-vivo, and secretes growth factors that promote angiogenesis (blood vessel formation). This makes adipose-derived mesenchymal stem cells an ideal potential therapy for chronic non-healing diabetic foot ulcers. Researchers are trying to develop strategies to ensure the viability and efficacy of MSCs in the hostile environment of ischemic tissue.
New Research into Diabetic Foot Wounds
The team at Assiut University is investigating whether a curcumin-loaded chitosan scaffold will be useful in stem cell therapy for ischemic foot wounds. Curcumin is a substance found in turmeric, a traditional Indian spice with powerful medicinal properties. Chitosan is a type of fiber found in crustacean shells. The question is whether this novel biocompatible and biodegradable scaffold will increase regenerative efficiency in ischemic wounds. The investigators will measure outcomes such as complete healing (full epithelization) of chronic diabetic foot wounds and the percentage of patients who achieve 50 percent wound closure in a period of six months. The rate of recurrence of ulcers after one year will also be reported. Approximately 40 patients with diabetes are expected to be enrolled in the study in October 2017 and the study will be completed in mid-2018.
References:
- https://clinicaltrials.gov/ct2/show/NCT03259217?term=stem+cells&sfpd_s=01%2F01%2F2017&sfpd_e=10%2F19%2F2017&draw=1&rank=1
- https://emedicine.medscape.com/article/460282-overview


