Hope to Patients with Rare Blood Disorder
Diamond Blackfan anemia (DBA) may not be widely known, but it is a very severe blood disorder that prevents bone marrow from producing enough red blood cells to carry oxygen throughout the body. Researchers at Boston Children’s Hospital’s Stem Cell Research Program recently completed a groundbreaking study aimed at developing potential treatments for this blood disorder.
Basic Facts About Diamond Blackfan Anemia
The body’s bone marrow serves the major purpose of producing blood cells, but Diamond Blackfan anemia (DBA) causes a bone marrow malfunction in which it cannot produce enough red blood cells. This stunts the body’s ability to carry oxygen to its own tissues, quickly causing fatigue, weakness, and pallor within the first year of life. Even worse, DBA puts the body at a much higher risk of developing serious complications as a result of malfunctioning bone marrow. These include myelodysplastic syndrome, a disorder that prevents blood cells from developing normally, as well as the cancer of blood-forming tissue called acute myeloid leukemia.
Due to the body function problems caused by DBA, people with the disease usually have specific physical abnormalities like unusually small head size, low front hairline, wide-set eyes, small lower jaw, cleft palate, malformed thumbs, and short stature. DBA is currently treated and managed with steroids, but the steroids only make a difference for half of all patients. Many patients eventually build up a tolerance to steroids and are forced to receive lifelong blood transfusions, leading to very poor quality of life.
Harnessing Induced Pluripotent Stem Cells (iPS) to Tackle DBA
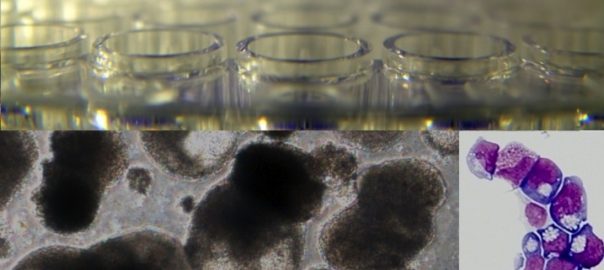
The team at Boston Children’s Hospital’s Stem Cell Research Program worked to find a more efficient treatment for DBA by converting some of the patients’ skin cells into induced pluripotent stem (iPS) cells. Induced pluripotent stem cells are adult stem cells genetically reprogrammed to enter an embryonic stem cell state, allowing them to be used to create virtually any cell or tissue in the body. This method of utilizing iPS to handle blood disorders marks a drastic change from past stem cell research, because “iPS cells have been hard to instruct when it comes to making blood. This is the first time iPS cells have been used to identify a drug to treat a blood disorder,” explained Sergei Doulatov, PhD, one of the authors of the study.
Once the team of researchers transformed the patients’ skin cells into iPS cells, they encouraged the iPS cells to make blood progenitor cells and put them through a rigorous drug screening system. Of the 1,440 chemicals tested in the system, one specific compound known as SMER28 successfully triggered mice and zebrafish to produce red blood cells. This means that SMER28, when used to treat the marrow in mice and zebrafish models of DBA, helps create red blood cells to stabilize or even reverse the severe anemia disease. Higher levels of SMER28 simply resulted in higher yields of red blood cells.
As the director of Boston Children’s Stem Cell Research Program, Leonard Zon, MD, stated, “It is very satisfying as physician scientists to find new potential treatments for rare blood diseases such as DBA.” Indeed, more research will continue to determine how the discoveries of this study can be applied to the human body in order to treat, reverse, or potentially cure DBA.
Image Source: https://vector.childrenshospital.org/


