Researchers Create Cells Resistant to HIV
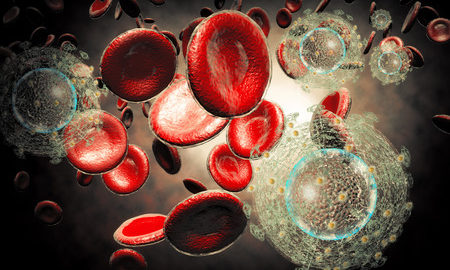
Researchers at The Scripps Research Institute, a not-for-profit biomedical research facility, have developed a new approach to make cells resistant to the HIV virus. In laboratory experiments, the HIV-resistant cells promptly replaced infected cells. The method offers a potential cure for people with HIV. The findings were published in Proceedings of the National Academy of Sciences.
Long-Term Protection and Cure for HIV
Senior staff scientist and co-author of the study, Jia Xie, explains the approach would offer long-term protection from the virus. In this method, antibodies to HIV are tethered to immune cells, thus creating a population of cells with resistance to the virus. When these resistant cells replace HIV-infected cells, the person with HIV could potentially be cured. The new therapy still needs to be tested for efficacy and safety before it can be used in patients.
Gene Therapy for AIDS
There are currently clinical trials underway at the City of Hope Center for Gene Therapy in California where investigators are studying whether transplantation of blood stem cells can help people with the disease. The newly discovered approach and study findings will be factored into ongoing trials with the ultimate goal that patients with AIDS can be treated by this method without needing other medications.
Researchers Create Cells Resistant to HIV
The new approach is a substantial technological advance over therapies that rely on free-floating antibodies in the patient’s bloodstream. These antibodies in the blood are present at relatively low concentrations. Antibodies that are tethered to the cell surface are better equipped to block virus access to critical cell receptors. Controlling the spread of HIV infection thus becomes easier. The scientists are calling it the neighbor effect, where one antibody stuck to the cell is far more effective than many antibodies present in the blood.
The experiments were conducted with rhinovirus models (which causes the common cold in many people). A vector known as lentivirus was used to deliver an antibody-synthesizing gene to cell cultures. These antibodies bound themselves to a receptor that is essential for the virus to spread. The tethered antibodies monopolized the receptor site and blocked the virus from entering the cell, thus controlling the spread of infection.
Study Findings for HIV-Resistant Cells
The investigators observed populations of engineered and non-engineered cells as well as a mixture of the two in the laboratory. When rhinovirus was first introduced, all cell populations suffered cell death. However, whereas the non-engineered cells never recovered, the engineered and mixed populations bounced back in number. In fact, compared to a control group that was not treated with rhinovirus, the engineered cell population returned to approximately the same number after 125 hours.
Further experiments consist of testing specialized antibodies from a library against the CD4 receptor of immune cells to which the HIV virus binds. Again, the fittest cells survived and the team ended up with a population of HIV-resistant cells in which the antibody had blocked the virus from binding to the CD4 receptor on immune cells.
References:
- https://www.medicalnewstoday.com/releases/316912.php


