Sickle Cell Treatment Shows Promise in Phase 1 Clinical Trial
The Dana-Farber/Boston Children’s Cancer and Blood Disorders Center have seen promising early results in a clinical trial to treat sickle cell disease. The first patient to undergo treatment has not received a blood transfusion in nine months, after receiving monthly blood transfusions for most of his life (1).
Sickle Cell Disease
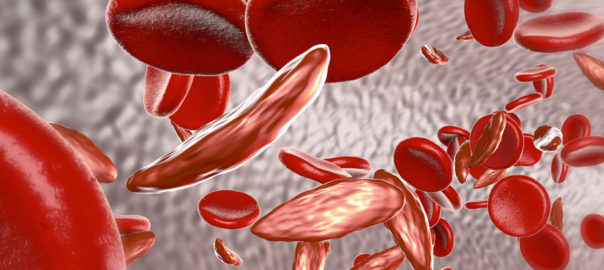
Sickle cell disease is a genetic disorder that affects the oxygen-carrying red blood cells. While normal red blood cells are shaped like the letter O, patients with sickle cell disease have red blood cells that are C shaped, stiff, and sticky. These red blood cells are more likely to cluster and form clots, leading to decreased oxygen delivery to organs. Additionally, sickle cell red blood cells are destroyed by the spleen much faster than healthy red blood cells, leading to anemia, a chronic lack of the oxygen-carrying cells in the blood. While there are many forms of sickle cell disease, the most common and most severe type is HbSS, which is one of the targets of the trial.
The Treatment
This trial is attempting to knock down expression of BCL11A, which represses the expression of fetal hemoglobin. By reducing BCL11A in hematopoietic stem cells (HSCs), the patient would produce fetal hemoglobin, which is not affected by the sickle cell mutation. To execute this trial, HSCs are removed from the patient and transduced with a lentiviral vector to express a short hairpin RNA that specifically targets BCL11A, which knocks down expression of the protein in these cells. The patients undergo chemotherapy to remove HSCs still present in the bone marrow and the modified HSCs are implanted and allowed to produce new blood cells (2).
Pre-clinical Trials
This therapy was first tested in animals to ensure safety and efficacy, and it was found that the treatment led to fetal hemoglobin levels reaching 80% levels of total hemoglobin. The reduction of sickle cell hemoglobin to below 20% is thought to prevent complications from sickle cell disease, such as strokes and other occlusions in blood vessels.
The Clinical Trial
The first patient, 21 year old Emmanuel “Manny” Johnson, underwent monthly blood transfusions since the age of 4, when the sickle cell trait led to him suffering two mild strokes. After undergoing treatment, he has not required a blood transfusion in 9 months. The treatment involved spending a month in the hospital undergoing chemotherapy and receiving the transplant of the genetically modified stem cells.
Manny credits his desire to help his brother Aiden, age 7, who also suffers from sickle cell disease. Manny is motivated to “do better for him” and hopes that the trial “can be an opening gate for many other kids and adults who are looking for a cure, looking for that life-changing factor.” The trial has enrolled additional patients and will begin expanding to treat teenage patients with sickle cell disease (1).
The Future
With current treatment options focused on preventing complications and treating the symptoms of sickle cell disease, this trial presents possibly the best opportunity to cure sickle cell disease. As the trial expands and patients move further along the treatment plan, increased data will bear out the possibilities and limitations with this treatment.
References
1. https://www.bostonherald.com/2019/01/27/brockton-brothers-with-sickle-cell-beat-the-odds/
2. http://www.danafarberbostonchildrens.org/innovative-approaches/gene-therapy/clinical-trials/sickle-cell-disease.aspx


