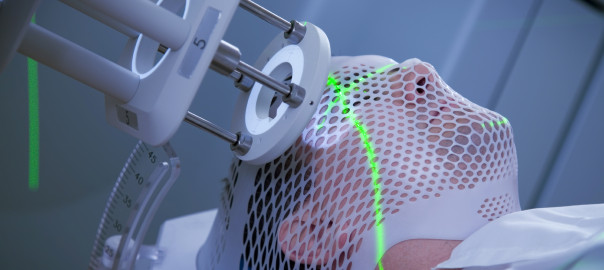
How Stem Cells Limit The Negative Effects of Brain Cancer Radiation
Stem cell therapy has already shown tremendous promise in healing areas of the brain damaged by radiation injury from cancer treatment. Scientists at the University of California Irvine have now made a promising discovery that an isolated part of stem cells called microvesicles can produce comparable benefits, without some of the risks associated with stem cells.
Microvesicles are tiny fluid-filled sac-like structures secreted by all human cells, including stem cells. Microvesicles play a critical role in tissue regeneration, because their plasma is rich in bioactive proteins and RNA necessary for cell physiology. In the brain, microvesicles ensure the healthy functioning of neurons.
Researchers, led by Professor Charles Limoli of the Department of Radiation Oncology at UCI, studied the effect of stem-cell-derived microvesicles in rats. When transplanted a couple of days following cranial irradiation, microvesicles were successful in restoring cognitive function, reducing the inflammatory response, and protecting neurons. When observed after four and six weeks, there was no sign of either tumor formation or immune-mediated rejection—the two major risk factors associated with stem cell therapy.
The study involved the isolation and extraction of microvesicles from multipotent human neural stem cells and their injection into the hippocampus (a region of the brain which rapidly produces new neurons) of rats that had undergone brain irradiation. When observed a month after irradiation, the rodents who had been treated showed that radiation injury had been either prevented or reversed, as demonstrated by the presence of considerably less inflammation, improved cognition (gauged from four different behavioral tasks), and preservation of the neuronal structure.
A similar study in 2011 at the same institution had looked at the use of multipotent human neural stem cells for this same purpose. But the results were burdened with unacceptable side effects such as immune-mediated rejections, altered growth of existing tumors, and concerns for teratoma formation. The strategy of using microvesicles has overcome these major issues.
Radiotherapy for brain tumors is limited by its side effects that can include anything from hair loss and tiredness to overall sickness and worsening of brain tumor symptoms. Memory loss and learning disability can greatly impact a patient’s quality of life, and the majority of people undergoing cranial irradiation experience severely debilitating cognitive impairment that is progressive with increasing doses of radiotherapy. The use of microvesicles can substantially lower these side effects, allowing the use of more aggressive radiotherapy to treat brain tumors.
Limoli indicates that further research is needed to identify the specific constituents of microvesicles that produce these beneficial effects. The longevity of neuro-protection afforded by the treatment also needs to be determined.
References:
https://www.sciencedaily.com/releases/2016/04/160407150628.htm
Image courtesy of http://arizonaoncology.com/


